3. Structure of PROMS. What outcomes are important?
Structure of PROMS. What outcomes are important?
PROs must be carefully defined so that they capture information that is important to patients. This information must also be measured accurately and – as much as possible – in a way that makes it comparable with other measurements.
Prior to going into more detail of PROs one should be familiar with the following (broad) definitions:
PRO Measure: Patient-reported outcome measures (PROMs) are standardised, validated questionnaires (which are also called instruments, scales or tools.) plus the information and documentation that support their use, completed by patients to capture their perception of their functional well-being and health status
PRO concept: The object of measurement, such as:
- a symptom or group of symptoms,
- effects on a particular function or group of functions, or
- a group of symptoms or functions shown to measure the severity of a health condition.
PRO domain: A sub concept represented by a score of a PROM that measures a larger concept comprised of multiple domains, such as for example:
Concept = Psychological state →Domain = Depression
PRO item: An individual question, statement, or task (and its standardised response options) that is evaluated by the patient to address a particular concept, such as:
Concept = Psychological state →Domain = Depression →Item = Are you feeling depressed?
Conceptual framework: The conceptual framework explicitly defines the concepts measured by the instrument in a diagram that presents a description of the relationships between items, domain (sub-concepts) and concepts measured and the scores produced by a PRO instrument (Figure 1 )
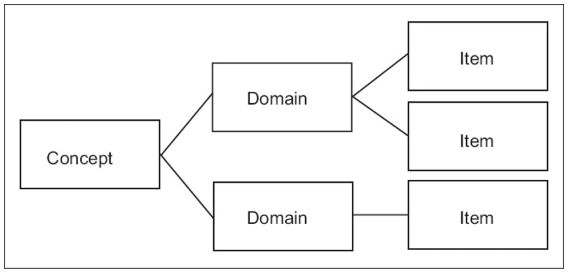
Figure. 1: Conceptual framework in PROM
Poor development of concepts may result in the measurement of outcomes that are not important to patients (however accurately measured), while poor measurement methods may identify an outcome that is important to patients, but difficult to interpret.
This means that how a question (item) is formulated is very important – vague questions may provide vague information; that is not useful. For instance, a patient may be asked, ‘How are you feeling on a scale of 1 to 10?’ (1 being poorly and 10 being extremely well). This is very vague. More specific questions relating to emotional wellbeing (concept) influenced by mobility, ease of breathing, etc. (domains), will provide more detailed and specific information. Deciding what to measure and how detailed a question must be formulated is therefore critical.
- It is important to distinguish the concept from the questions that you need to ask to detect and assess a change in the concept.
For example, investigators researching the response of patients with COPD to a therapy may recognise that these patients may find performing tasks more difficult in the morning. The concept that they decide to measure is the burden and extent of morning symptoms and the ability of patients to perform activities at that time of day. The items to capture this concept may be questions such as:
- Did you wash yourself this morning other than your face, i.e. body wash, shower, bathe?
- Did you get dressed this morning?
- Did you walk around your home early this morning after taking your medicine?
The optional answers that patients are given to these questions may include a range of responses, such as:
- Yes, I did it myself.
- Yes, but I needed help.
- No, I was unable to.
- No, I did not for other reasons.
Patients may also be given an option to respond to a follow up question, such as ‘How difficult was it for you to perform this task?’
In some cases, caregivers or healthcare professionals have developed the concept attached to a disease and patient group. However, the need for patients themselves to help identify and develop concepts has become increasingly recognised. Table 1 contains a list with descriptions of the major concepts addressed by PROs.
The most commonly used PRO questionnaires assess one of the following constructs:
Table 1: Major concepts measured in PROs
|
Concept |
Description |
|
Quality of life (QoL) |
The World Health Organization (WHO) defines QoL as "an individual 's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns". Standard indicators of the quality of life include wealth, employment, the environment, physical and mental health, education, recreation and leisure time, social belonging, religious beliefs, safety, security and freedom. QoL has a wide range of contexts, including the fields of international development, healthcare, politics and employment. |
|
Health-Related Quality of life (HRQoL) |
HRQoL is multi-dimensional; it represents the patient's evaluation of a health condition, and its treatment, on their daily life, including: physical function, psychological function, social function, role function, emotional function, well-being, vitality, health status, etc. HRQoL is an evaluation of QoL and its relationship with health. |
|
Patient satisfaction (Reports and Ratings of health care) |
Evaluation of treatments, patient’s preference, healthcare delivery systems and professionals, patient education programmes, and medical devices. |
|
Physical functioning (disability) |
Physical limitations and activity restrictions, including: self-care, walking, mobility, sleep, sex, disability. |
|
Psychological state |
Positive or negative affect and cognitive functioning, including but not limited to: anger, alertness, self-esteem, sense of well-being, distress, coping, feeling anxious or depressed. |
|
Signs and symptoms (impairments) and other aspects of well-being |
Reports of not directly observable symptoms or sensations, including: energy and fatigue, nausea, irritability. |
|
Social functioning |
Limitations in work or school, participation in community. |
|
Treatment adherence |
Reports or observations of actual use of treatments. |
|
Utility, or usefulness, is the (perceived) ability of something to satisfy needs or wants. In health economics, utilities measure the strength of patient preferences. For example, how important various factors are to patients, such as symptoms, pain, and psychological health. The impact of new treatments on those factors, and therefore on quality of life (QoL), can then be calculated. This is a common approach used by health technology assessment (HTA) bodies, which advise on whether treatments should be funded by e.g., government health departments. (See box on Health Utility Measures in lesson 6) |
Adapted from: https://eprovide.mapi-trust.org/about/about-eprovide