4. EudraVigilance
1. EudraVigilance
1.3. Reports
1.3.1 Electronic reporting
Data in EudraVigilance is submitted electronically by national regulatory authorities and by marketing authorisation holders for medicines. Electronic reporting and evaluation of suspected ADRs is obligatory for MAHs and NCAs[1] and covers elements as shown in the following table (Table 1):
Table 1: Electronic reporting obligations in the EU; adapted from Eudravigilance-electronic-reporting
|
From where |
Who |
What |
|
Interventional clinical trials |
· Marketing authorisation holders
|
Reports of suspected unexpected serious adverse reactions (SUSARs) via safety reports in clinical trials (individual case safety reports (ICSRs)) |
|
• Marketing authorisation holders • Sponsors of clinical trials |
Information on investigational medicinal products via product reports (for Article 57 database) |
|
|
Spontaneous reports [2] and non-interventional studies |
|
Reports of suspected adverse reactions for authorised medicinal products via safety reports (ICSRs): - suspected serious adverse reactions occurring within and outside the EEA - suspected non-serious adverse reactions occurring within the EEA |
|
Marketing authorisation holders |
Information on authorised medicinal products via product reports (for Article 57 database) |
Patients, consumers and healthcare professionals (HCPs) can report, and are encouraged to do so, suspected adverse reactions to either the national competent authorities or the marketing authorisation holders of the medicine. These reports are then transmitted electronically and stored in the EudraVigilance database.
Background
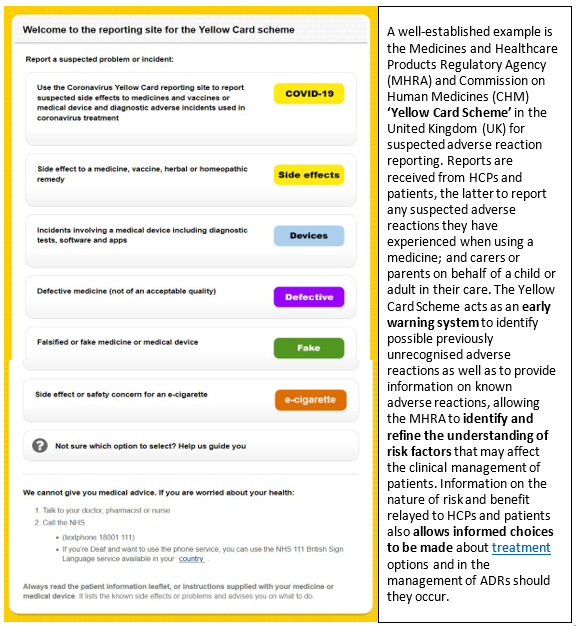
Recognition by health authorities of the advantages of complementing reports on suspected adverse reactions from HCPs with those from patients triggered a number of changes to existing pharmacovigilance systems in Europe. In 2003, Denmark and the Netherlands became the first countries to allow patients and consumers to report suspected adverse reactions directly to their regulatory authority, followed by Italy (2004), the United Kingdom (2005) and Sweden (2008)[3] An example from the UK is shown in the following figure (Fig. 2)
Since 2012, with new EU pharmacovigilance legislation, patient reporting has been expanded throughout the EU. Member States are now mandated to encourage patients to report suspected adverse reactions directly to the regulatory authority and to enable reporting through web-based formats and alternative means. Likewise, marketing authorisation holders (MAHs) shall record all suspected adverse reactions, whether reported spontaneously by patients or healthcare professionals and not refuse to consider adverse reaction reports received from patients through appropriate means and shall ensure that those reports are accessible at a single point within the Union.[4]
By introducing a legal right for patients to report suspected ADRs directly to regulatory authorities, the EU acknowledges patients and consumers as key sources of information on medicines safety and fosters faster and more comprehensive collection of data on adverse reactions.
To note:
In spite of the fact that spontaneous reporting is crucial for signal detection, under-reporting is common. It is estimated that only 1% to 10% of serious adverse reactions are reported [5] . Healthcare professionals often attribute low reporting to lack of time and sometimes only report adverse reactions when convinced of a causal association between a medicine’s use and an adverse reaction [6]. Additionally, whilst patients consider certain ADRs to be very significant in affecting their quality of life, healthcare professionals do not to the same extent [7] .
The added value of patients’ reporting is that their reports tended to be more elaborate in description of suspected ADRs by including detailed descriptions of symptoms and the social, emotional and occupational impact. According to an evaluation of patient reporting to the Yellow Card Scheme [8], patients report a different spectrum of reaction types compared with healthcare professionals, although there is a reasonable amount of overlap. Because the patient focus in the reports differs from healthcare professionals, patient reporting of suspected ADRs has the potential to add considerable value to pharmacovigilance. They can generate new potential safety signals and describe suspected ADRs in enough detail to provide useful information on the likely causality and the impact on patients' lives.
Patients are more likely than healthcare professionals to report:
- Symptoms (93% vs 78%).
- Impact of the ADR (47% vs 12%).
- Temporal relationship between medicine and suspected ADR.
- Extreme nature of the suspected ADR (47% vs 17%).
Pharmaceutical companies holding or applying for a marketing authorisation in the European Economic Area (EEA), sponsors of clinical trials and NCAs in the EEA need to register with EudraVigilance for the electronic data interchange of pharmacovigilance information (see box below). The registration process is a prerequisite also for electronic reporting. All users, including organisations, need an active EMA account created through the EMA Account Management portal.
|
Registration is mandatory for:
|
[1]
DIRECTIVE 2001/83/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 6 November 2001 on the Community code relating to medicinal products for human use (consolidated 2019) Art.107, 107a.
https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:02001L0083-20190726&from=EN
[2] Spontaneous reports are unsolicited reports by healthcare professionals or patients that do not derive from a study or any organised data-collection scheme. https://www.adrreports.eu/en/background.html
[3] Herxheimer, A, R Crombag, and TL Alves. "Direct f reporting of adverse drug reactions. A twelve-country survey; literature review." Health Action International Europe. May 2010.https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:02001L0083-20190726&from=EN
[6] Herdeiro, Maria T et al. "Physicians’ Attitudes to Adverse Drug Reaction Reporting. A case control study in Portugal" Drug safety 28.9 (2005): 825-833.
[7] Frankenfeld, Christian. "“Serious” and “severe” adverse drug reactions need defining." BMJ 329.7465 (2004): 573.
[8] Avery AJ, Anderson C, Bond CM, Fortnum H, Gifford A, Hannaford PC, et al. Evaluation of patient reporting of adverse drug reactions to the UK Yellow Card Scheme: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess 2011; 15 (20).http://www.ncbi.nlm.nih.gov/pubmed/21545758