What is pharmacovigilance (PhV)?
3. EU Pharmacovigilance – objectives - aims - tasks
Following the above definition of pharmacovigilance, according to the EMA the underlying objectives of the applicable EU legislation for pharmacovigilance are:
- preventing harm from adverse reactions in humans arising from the use of authorised medicinal products within or outside the terms of marketing authorisation or from occupational exposure;
- promoting the safe and effective use of medicinal products, in particular through providing timely information about the safety of medicinal products to patients, healthcare professionals and the public.
Specific aims of pharmacovigilance are to:
- Maintain a robust monitoring system for new safety issues.
- Implement effective approaches to minimise risk.
- Install procedures for rapid decision making and triggering actions in case of (immediate) safety concerns
- Improve patient care and safety in relation to the use of medicines and all medical and paramedical (services that support medical work, such as nursing, first aid, radiography) interventions.
- Improve public health and safety in relation to the use of medicines.
- Contribute to the assessment of benefit, risk, and effectiveness (including cost-effectiveness) of medicines.
- Secure the accessibility of information about the safety of medicinal products to patients, healthcare professionals and the public.
- Promote understanding, education and training in pharmacovigilance and its effective communication to the public.
- Monitor impact of measures and activities and ensure continuous improvement of pharmacovigilance system
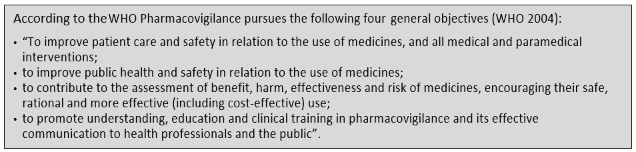
The above list incorporates what the WHO calls the general objectives.
Pharmacovigilance is therefore an activity
contributing to the protection of patients’ and public health.
Main pharmacovigilance related tasks:
The pharmacovigilance process can be broken down into the following key tasks:
- Assessing the known and potential risks of each medicine before marketing and developing plans to collect data and minimise those risks (risk management planning); (See lesson 2 on risk management)
- Collecting and managing data of possible adverse reactions (ADR); (see section 2 below on ADRs)
- Signal detection and management - analysing the data (reports of suspected adverse reactions) to identify ‘signals’ (any new or changing safety issue); (see section 1.5 on Signals)
- Routine benefit-risk monitoring of medicines via periodic safety update reports (PSURs).
Europe-wide reviews and evaluation of important safety and benefit-risk issues and decision on whether and which (regulatory) action to take; e.g., PhV referrals (in a referral procedure, the EMA is requested to conduct a scientific assessment of the safety concern for the EU).
- Acting to protect public health (including regulatory action).
- Managing information on products under additional monitoring, and products that have been withdrawn.
- Identifying and reducing the risk of medication errors before and after the authorisation of a medicine.
- Assessing and co-ordinating studies after marketing through post-authorisation safety studies and post-authorisation efficacy studies.
- Carrying out inspections to ensure company pharmacovigilance systems comply with good pharmacovigilance practice.
- Communicating in a clear, effective and timely manner about safety-related issues to relevant stakeholders.
- Interacting with and engaging key stakeholders, including patients, healthcare professionals, the pharmaceutical industry, other parts of the regulatory system (including international regulators), academia, the media, and wider civil society
- Monitoring performance of the system and its components, including compliance with legal obligations and standards.
- Continuous development and improvement of systems (including IT infrastructure), guidelines and standards, and promotion of research to address knowledge gaps.