Bias in Clinical Trials
Completion requirements
View
1. Where Bias Can Be Introduced
1.3. During Trial Conduct
There are a few common problems that may arise during the course of a trial related to participant adherence (compliance) to the protocol and to the prescribed treatment schedule. For example:
- Participants may turn out to be ineligible after randomisation.
- Treatment may have been interrupted or modified but not according to the rules specified in the protocol.
- Disease assessments may have been delayed or not performed at all.
- A participant may decide to stop taking part in the trial, etc.
This can be problematic if not properly accounted for in the analysis. For example, consider the setting of a clinical trial comparing a new experimental treatment to the standard of care. In this trial some participants taking the experimental treatment are too sick to go to the next visit within the allotted time due to side effects. A possible approach would be to include only participants with complete follow-up, so to exclude the sick participants from the analysis. However, by doing so, one selects a sub-group of patients whom, by definition, will present an artificially positive picture of the treatment under trial. This is again an example of selection bias.
One potential solution to this problem is a statistical concept called an intention-to-treat (ITT) analysis. ITT analysis includes every randomised patient whether they received the treatment or not. As such, ITT analyses maintain the balance of patients' baseline characteristics between the different trial arms obtained from the randomisation. ‘Protocol deviations’ such as non-compliance to the assigned treatment (schedule, dosing, etc.) are part of daily practice. Therefore, treatment-effect estimates obtained from ITT analysis are considered to be more representative of the actual benefit of a new treatment
Bias can also happen when measuring the endpoint(s) of interest. For instance, time to disease progression or relapse can be severely affected by the hospital visit schedule. The frequency of disease assessment should be adequate and frequent enough to capture correctly the events that could not be observed by means other than by medical examination at the hospital. The disease assessment schedules should also be the same in both arms.
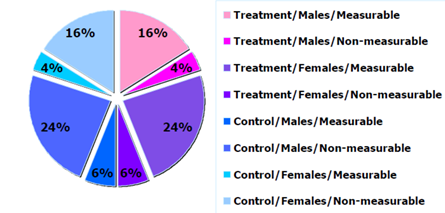
Figure 3: Example of sample distribution by arm and sex.