1. Cohort studies
1.2. Prospective cohort studies: Points to consider
Advantages
- the only observational study design that directly investigates risk of disease and the factors contributing to it
- allows examination of multiple outcomes of a single exposure
- good for rare or unusual types of exposures, e.g., contact with a chemical spill in a factory, unusual occupational exposures (e.g., asbestos, or solvents in chemical manufacturing)
- best for common outcomes
- ethically safe
- advantage over retrospective cohort and case control studies because baseline exposure status is correctly assessed, not only recalled
- clarity of temporal sequence (Did the exposure precede the outcome?): since at the time of entry into the cohort study, when their exposure status is established, individuals do not have the outcome, more clearly indicates the temporal sequence between exposure and outcome, gives some indication of causality
- accurate measurement of exposure variable, other variables, and outcomes: may help in reducing the bias in measurement of exposure
- can measure the change in exposure and outcome over time
- yield true incidence rates and relative risks
- may uncover unanticipated associations with outcome
- avoid selection bias at enrolment: reduces the possibility that the results will be biased by selecting subjects for the comparison group who may be more or less likely to have the outcome of interest, because the outcome is not known at baseline when exposure status is established.
Drawbacks
- data analysis needs sufficient follow-up time after study start, therefore not appropriate for rare outcomes/diseases or those that take a long time to develop (long latency)
- can be costly and time consuming
- not appropriate for studying multiple exposures[1]
- confounding factors within the sample groups may be difficult to identify and control for, thus influencing the results, e.g. non-random allocation of exposure: possibility that the association found may be explained by other variables that differ between exposed and non-exposed participants and that also have an association with the outcome studied. If these other variables were measured, they can be adjusted for in the analysis, but frequently these factors are unmeasured, measured imprecisely, or even unknown
- participants moving between exposure/non-exposure categories or not properly complying with methodology requirements
- if a significant number of participants are not followed up (lost, death, dropped out) this may impact the validity of the study and may decrease the study’s power, and introduce so called attrition bias – a significant difference between the groups of those that did not complete the study
Key Concept: The distinguishing feature of a prospective cohort study is that at the time that the investigators begin enrolling participants and collecting baseline exposure information, none of the participants has developed any of the outcomes of interest, and eventually, an association between exposure and subsequent outcome can be established.
Example: The Nurses’ Health Study, the Nurses’ Health Study II and the Nurses’ Health Study III are well-known cohort studies established in 1976, 1989, and 2010 respectively, that have followed over 100,000 nurses. Participants are sent detailed questionnaires every two years. The nurses report information on their diet, lifestyle, medicines, family history, work arrangements, family life, etc. They also report on any diseases that they develop. The studies revealed many correlations between environmental factors and risks for health conditions in diverse topics and has resulted in hundreds of scientific papers and extensive press coverage[2].
This exemplary study is shown in the following figure (Fig. 3). To note: the graph illustrates one of the subgroups from this large single group study addressing a question in a specific area. Participants with the hypothesised risk factor are assigned to one group (exposed), the comparison group is comprised of participants without this risk factor but otherwise similar (internal control).
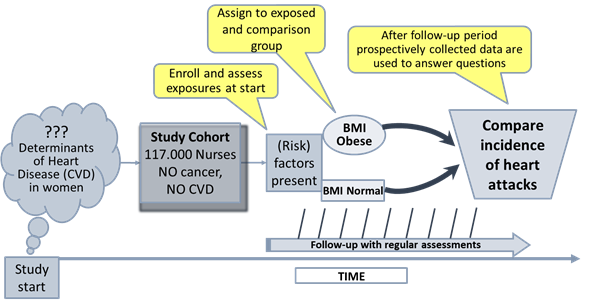
Figure 2: Schematic of a subgroup from the Nurses’ Health Study
addressing a specific question.
(BMI: Body Mass Index; 18,5-24,9 normal weight; 30-39,9 obese; CVD:
Cardiovascular Disease). Adapted from: https://sphweb.bumc.bu.edu/otlt/mph-modules/ep/ep713_analyticoverview/EP713_AnalyticOverview3.html
[1] However looking at different exposures in the same cohort would be possible as you could split the cohort based on different exposures (e.g. one analysis looking at the impact of BMI, another analysis of the same cohort looking at smoking, a third analysis looking at living in rural vs non-rural areas, etc.). This will increase the complexity and risks that the cohort subgroups become relatively small. You may also increase confounding.
[2] Nurses‘ Health Study https://www.nurseshealthstudy.org/