5.2. Types of Observational Studies: Case-control studies
| Site: | EUPATI Open Classroom |
| Course: | Epidemiology and Pharmacoepidemiology |
| Book: | 5.2. Types of Observational Studies: Case-control studies |
| Printed by: | Guest user |
| Date: | Tuesday, 3 June 2025, 3:20 AM |
1. Case-control studies
(This section is organised in the form of a book, please follow the blue arrows to navigate through the book or by following the navigation panel on the right side of the page.)
Case-controlled studies
are studies which involve identifying individuals who have the outcome/disease
of interest (cases) and matching them with individuals who have similar
characteristics, but do not have the outcome of interest (controls). Data about
exposure of interest (i.e., the hypothesised causal or contributing factors)
are then collected retrospectively, typically by interview, extracted from
records, or survey. Case-control studies assess whether there is a
statistically significant difference in the rates of exposure to the risk
factor(s) between the groups. This can suggest associations between the risk
factor(s) and development of the disease in question, although no definitive
causality can be determined. The main outcome measure in case-control studies
is the odds ratio (OR).
It is imperative that defined inclusion and exclusion criteria prior to the selection of cases are formulated to best ensure that all cases included in the study are based on the same diagnostic criteria. Cases should be selected from a reliable source such as a disease registry. Regardless of how the cases are selected, they should be representative of the broader disease population to support generalisability.
A particular problem in case-control studies is the selection of a comparable control group. Since the validity of the study depends upon the comparability of these two groups, principally, the distribution of exposure should be the same among cases and controls; in other words, ideally both, cases and controls, should come from the same source population. For example, if cases are selected from a defined population such as a general practitioner (GP) register, then controls should comprise a sample from the same GP register.
Investigations examining rare outcomes may have a limited number of
cases to select from, whereas the source population from which controls can be taken
is much larger. In such scenarios, the study may be able to provide more
information if multiple controls per case (about three or four) are added thus
increasing the sample size. Also, matching controls to the selected cases on
the basis of various factors (e.g., age, sex) is a possibility to prevent
confounding of the study results. Matching may even increase the “statistical
power” and precision of the study.
1.1. Bias in case-control studies
Retrospective studies, and in particular case-control studies, are susceptible to the effects of bias, which may be introduced during the collection of exposure and outcome data. Three kinds of bias are predominant and are briefly described in the following. Bias decreases the internal validity of the investigation and should be addressed and reduced in the study design as there are limited options for the control of bias during the analysis.
Recall bias: When information about exposure is collected by self-report, it is susceptible to recall bias. Recall bias occurs e.g., when a differential response between cases and controls occurs. The common scenario is when a participant with disease (case) will unconsciously recall and report an exposure with better clarity due to the disease experience.
Interviewer/observer bias Interviewer bias occurs when the interviewer asks leading questions or has an inconsistent interview approach between cases and controls or the interviewer’s knowledge of an individual's disease status is insufficient. A good study design will implement a standardised interview in a non-judgmental atmosphere with well-trained interviewers to reduce interviewer bias.
Selection bias: Selection bias is a particular problem in case-control studies, leading to non-comparability between cases and controls when cases (or controls) are included in, or excluded from a study because of some characteristic they show, related to exposure to the risk factor under evaluation. It may occur when those individuals selected as controls are unrepresentative of the population providing the cases. Selection bias may also be introduced when exposed cases are more likely to be selected than unexposed cases. The potential for selection bias may be minimized by selecting controls from more than one source, such as by using both hospital and neighbourhood controls.
1.2. Case-Control Studies: Points to consider
Retrospective cohort studies are NOT the same as case-control studies: Cohort studies start out by classifying a group of people according to an exposure. Then, the investigator determines whether the exposed and unexposed people develop a disease or not. Case-control studies first identify a group of people with a disease. Then the investigator selects a comparison or control group without the disease. The two groups are compared and analysed for exposures. Because case-control studies begin with people who are sick or not sick, and examine previous exposures, they are retrospective.
Advantages
- can examine rare outcomes or outcomes with long latency because subjects are selected from the outset by their outcome status and the analysis is retrospective
- relatively quick to conduct
- relatively inexpensive to perform
- require comparatively few subjects
- existing records can be used
- multiple exposures or risk factors can be examined for one outcome, enabling a better understanding of possible risk factors for the outcome / disease
- no ethical issues in terms of collecting data if legally accessible
- many aetiological factors can be observed at the same time
- no need for follow up
Drawbacks
- particularly prone to recall bias
- difficult to validate information
- control of extraneous variables difficult and may be incomplete
selection of an appropriate comparison group cumbersome
- can only assess one
outcome within one analysis
- cannot establish prevalence
- quality of historic data often insufficient
Example: A paediatrician wants to study the association between the use of tap water for drinking and diarrhoea. His hypothesis is that “children using tap water for drinking are more likely to suffer from diarrhoea as compared to those who use mineral water”. In this example children who are suffering from diarrhoea will be cases while those not having diarrhoea will be controls. The exposure in this study is the use of tap water for drinking while the outcome is diarrhoea. Cases and controls are questioned, or their medical records are consulted regarding past exposure to risk factors (in this example tap water).
Later measure of association is determined which in a case-control study is “Odd Ratio” (K Park, 20th edition).
Example: Another case-control study design is by Chung[1] and colleagues, who examined maternal cigarette smoking during pregnancy and the risk of new-borns developing cleft lip/palate. A salient feature of this study is the use of the 1996 U.S. Natality database, a population database, from which both cases and controls were selected. This database provides a large sample size to assess new-born development of cleft lip/palate (outcome), which has a reported incidence of 1 in 1000 live births, and also enabled the investigators to choose controls (i.e., healthy new-borns) that were generalizable to the general population to strengthen the study's external validity. A significant relationship with maternal cigarette smoking and cleft lip/palate in the new-born was reported in this study (adjusted Odds ratio (OR) 1.34, 95% Confidence Interval (CI) 1.36-1.76). You can find more information about Odds ration in Statistics course.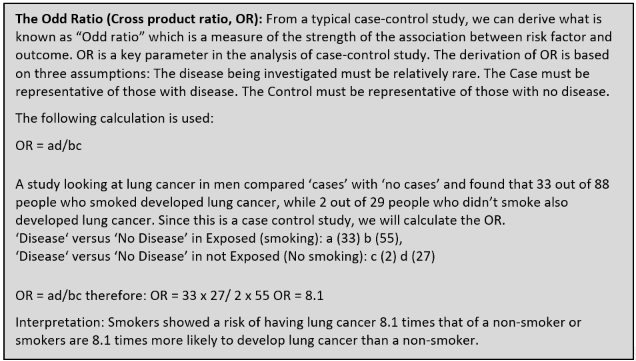
[1] Chung KC, Kowalski CP,
Kim HM, Buchman SR. Maternal cigarette smoking during pregnancy and the risk of having a
child with cleft lip/palate. Plast Reconstr Surg. 2000 Feb;105(2):485-91. doi:
10.1097/00006534-200002000-00001. PMID: 10697150.
https://pubmed.ncbi.nlm.nih.gov/10697150/