Synthetic Chemical Medicines
2. How do chemical medicines work?
After chemical medicines are taken (e.g. by being swallowed, absorbed through the skin, inhaled or injected), the active ingredient of the medicine enters the circulation and is carried in the blood to the intended target. Once it has reached the part of the body where it is needed, it will interact with the local cells to produce the desired effects.Most chemical medicines are recognised by a specific type of cell and will either act on the cell surface or will be taken inside the cell. This occurs because the cells in our bodies have molecules on the surface called receptors. Medicines attach to their target receptors, much like a key fit into a lock, and this triggers a response in the cell, resulting in the turning on (stimulation) or turning off (inhibition) of an effect (Figure 2).
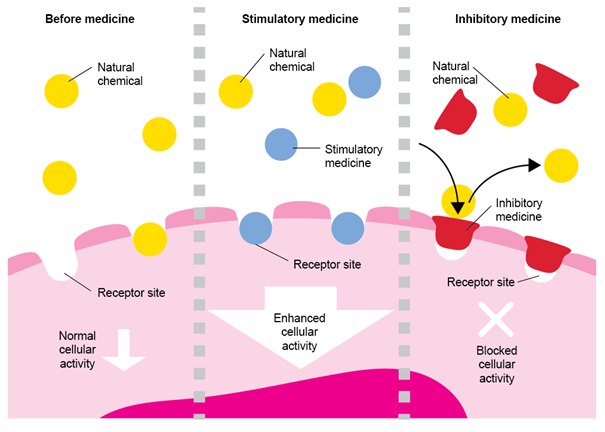
Figure 2. Active substances bind to cell receptors and enhance cellular activity by continually occupying receptors. Similarly, this can cause blockade of cellular activity by preventing the natural chemical from binding to the receptor .
Some medicines work in the same way as molecules naturally occurring in the body, for example, morphine and similar medicines mimic the actions of endorphins (chemicals produced naturally in the body to reduce pain). Morphine can reduce pain by binding to the same receptors as endorphins. Pain is felt because cells in the nervous system send pain signals to the brain, usually because of injury or illness. By binding to pain receptors on cells of the nervous system, morphine can instruct them to turn off the pain signals.
Other medicines work by blocking the receptors on cells, so that naturally occurring molecules cannot exert their normal effect. An example of this is the family of medicines called beta-blockers, which are used to treat heart conditions and other illnesses. In normal circumstances, the hormones adrenaline and noradrenaline are released in times of stress and, by binding to the beta receptors, they can overstimulate the heart. When a patient at risk of high blood pressure or a heart attack takes a beta blocker, the medicine binds to beta receptors and blocks them, meaning that adrenaline and noradrenaline cannot reach the receptors and overstimulate the heart.
Some medicines attach to only one type of receptor, but others can attach to several different types of receptors throughout the body, which often explains how effective each medicine is in reaching its target. Medicines that are very specific to one receptor often have a better side-effect profile than medicines that are less specific. Even for very specific medicines, binding to the receptor is temporary and, after a while, the molecules will let go of the receptor and leave the body. A new dose may be needed to continue the medicine’s effect, which is why many medicines are given with instructions about how often they should be taken.