Risk Factors in Health and Disease
| Site: | EUPATI Open Classroom |
| Course: | Predisposing Factors and Underlying Mechanisms of Disease |
| Book: | Risk Factors in Health and Disease |
| Printed by: | Guest user |
| Date: | Friday, 13 June 2025, 12:38 PM |
1. What are risk factors?
(This section is organised in the form of a book, please follow the blue arrows to navigate through the book or by following the navigation panel on the right side of the page.)
Ageing populations and longer life expectancy have led to an increase in long-term (chronic), expensive-to-treat diseases and disabilities. However, there are not enough healthcare resources to cope with this rising demand. This puts the healthcare sector under increasing budget pressure. It is important that we, as a society and users of healthcare systems, understand the causes and risk factors behind these diseases so that we can actively take part in cost effective prevention and treatment programmes. Health and wellbeing are affected by many factors – those linked to poor health, disability, disease or death are known as risk factors.
A risk factor is a characteristic, condition, or behaviour that increases the possibility of getting a disease or injury. Risk factors are often presented individually, however in practice they do not occur alone. They often co-exist and interact with one another.
For example, physical inactivity will, over time, cause weight gain, high blood pressure and high cholesterol levels. These significantly increase the chance of developing chronic heart diseases and other health related problems.
In general, risk factors can be categorised into the following groups:
- Behavioural
- Physiological
- Demographic
- Environmental
- Genetic.
These are described in more detail below.
Behavioural risk factors usually relate to ‘actions’ that the individual has chosen to take. They can therefore be eliminated or reduced through lifestyle or behavioural choices. Examples include:
- smoking tobacco
- drinking too much alcohol
- poor diet and nutrition
- physical inactivity
- spending too much time in the sun
- not having certain vaccinations
- unsafe sex
Physiological risk factors are those relating to an individual’s body or biology. They may be influenced by a combination of genetic, lifestyle and other broad factors. Examples include:
- being overweight or obese
- high blood pressure
- high blood cholesterol
- high blood sugar (glucose).
Demographic risk factors are those that relate to the overall population. Examples include:
- age
- population subgroups such as occupation, religion or income.
Environmental risk factors cover a wide range of topics such as social, economic, cultural and political factors as well as physical, chemical and biological factors. Examples include:
- access to clean water and sanitation
- risks in the workplace
- air pollution
- social relationships.
Genetic risk factors are based on an individual's genes. Some diseases, such as cystic fibrosis and muscular dystrophy, come entirely from an individual's ‘genetic make-up’. Many other diseases, such as asthma or diabetes, reflect the interaction between the genes of the individual and environmental factors.
2. Global Risk for Mortality
Table 1: WHO numbers of the 10 leading global risks for mortality (death), 2004
|
Rank |
% of total deaths |
|
|
1 |
High blood pressure |
12.8 |
|
2 |
Tobacco use |
8.7 |
|
3 |
High blood glucose |
5.8 |
|
4 |
Physical inactivity |
5.5 |
|
5 |
Overweight and obesity |
4.8 |
|
6 |
High cholesterol |
4.5 |
|
7 |
Unsafe sex |
4.0 |
|
8 |
Alcohol use |
3.8 |
|
9 |
Childhood underweight |
3.8 |
|
10 |
Indoor smoke from solid fuels |
3.3 |
The number of total global
deaths in 2004 was 59 million people.
Table 1 shows the 10 most common risk factors that caused a large portion of total global deaths in 2004 according to the World Health Organisation (WHO). The top six leading risk factors are all linked to potential development of long-term diseases, such as heart disease, diabetes and cancers.
The ranking seen in Table 1 differs if income and other demographic factors are considered.
For high- and middle-income countries, the most important risk factors are those related to long-term diseases whereas in low-income countries, factors such as childhood malnutrition and unsafe sex are much more widespread.
Risk factors also change with age. Some risk factors almost exclusively affect children such as malnutrition and indoor smoke from solid fuels. For adults, there are considerable differences depending on age:
- Unsafe sex and addictive substances (e.g. tobacco and alcohol) account for most of the health problems in younger adults
- Risk factors for long-term diseases and cancers mainly affect older adults.
Gender differences also exist. For example, men are much more likely to be at risk of factors associated with addictive substances. Women during pregnancy often suffer from iron deficiency.
3. Reducing Exposure to Risk Factors
Reducing contact (exposure) to risk factors would greatly improve global health and life expectancy by many years. This would therefore reduce healthcare costs.
One good example demonstrating this is ‘The Systematic COronary Risk Evaluation Project’ (The SCORE project). The SCORE project data are based on national data sets from Europe, totalling around 250,000 people with around 3 million patient-years of follow-up. The SCORE risk assessment is a simple tool to predict deaths relating to heart or circulation problems (fatal cardiovascular disease, CVD) over a 10-year period.
It is based on the following risk factors:
- Gender
- Age
- Smoking habits
- Systolic blood pressure
- Total cholesterol levels.
The threshold for being at high risk is defined as ≥ 5% (greater than or equal to 5 per cent); this means that 5 or more out of 100 people will die within 10 years.
4. Example: SCORE
A 40-year-old man, who is a smoker, visits his doctor for a routine health check. The checks show the following:- His blood pressure is 160/90 (mm Hg) - a normal range of blood pressure is 90/60 to 140/90 (mm Hg).
- His cholesterol level is 8 (mM/L) - a normal cholesterol level is less than 5.2 (mM/L).
By applying these data to the SCORE chart (see Figure 1) it turns out that his risk of getting a fatal CVD is 3% over a 10 year period. Suppose this man does not change his habits and continues with the same lifestyle pattern. It can be projected that at an age of 60 his risk for having a fatal CVD has increased dramatically to 24%. In other words, 24 out of 100 people with this risk will die.
Based on these findings the doctor and the 40-year-old man should agree preventative actions to improve his health status, such as:
- Dietary advice
- Plan for physical activity
- Help to stop smoking and
- Prescription of medicines.
Let us say they agree on a plan and the 40-year-old man follows this. He changes his lifestyle and comes back at the age of 60. He is a non-smoker with the following health data:
- His blood pressure is now 140/80 (mm hg) - this is within a normal range.
- His cholesterol level has dropped to 5 (mM/l) - this is within a normal range.
By using the SCORE chart (see Figure 1), his risk of getting fatal CVD is now 5%, which is much better than the 24% projected if he had continued his former lifestyle. It is important that he continue to follow the healthy lifestyle he has adopted in order to minimise the risk of getting fatal CVD as he gets older.
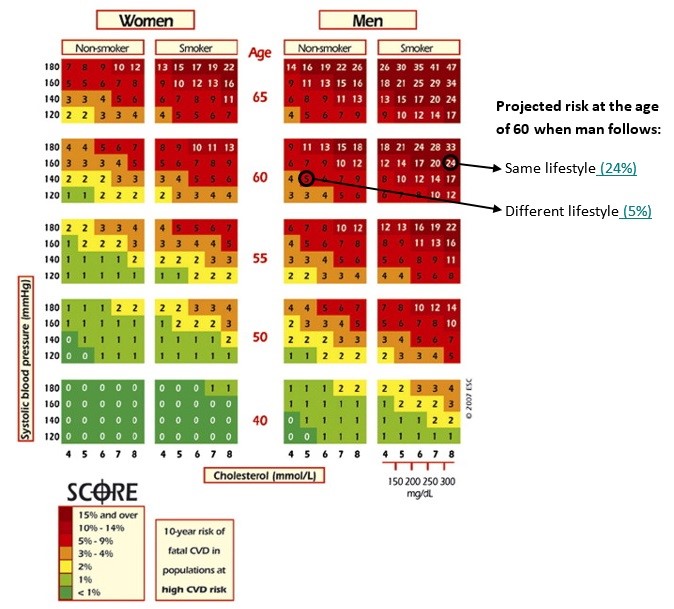
Figure 1: SCORE chart to predict the total risk over a 10 year period for fatal CVD based on gender, age, smoking habits, systolic blood pressure and total cholesterol levels (Source: European Society of Cardiology).
This example shows how the different factors such as gender, age, smoking habits, cholesterol levels and blood pressure influence the risk of a fatal CVD. By using this SCORE chart the doctor can show the patient a visual representation of what may happen over time. The patient and doctor can then work together to develop a plan. If followed, this can lead to significant improvement of the influencing factors, thereby reducing the risk of a fatal CVD.