Mechanisms of disease
2. Disease
2.3. Factors Causing a Disease
The factors causing a disease can be categorised into the following groups:
- External factors
- Internal factors
- Physiological factors
- Stress factors
- Susceptibility
These are described in more detail below.
External factors
The external factors causing imbalances or diseases include:
- Microbes (bacteria and viruses) and parasites (e.g. malaria and amoebae)
- Injuries (accidents)
- Environmental impact during an individual’s lifetime - this is also linked to personal habits mentioned as ‘lifestyle’, e.g. food and fluid intake and physical exercise.
Internal factors
These are also known as ‘genetic factors’. If the genes of the sexual organs (i.e. egg or sperm) are permanently harmed by external factors, a change in the genes (‘mutation’) can appear. This may cause ‘monogenetic disease’ in the offspring - this is disease caused by a single defective gene. Sometimes this is easily observed (e.g. in dwarfism, where people are short in stature), where for others it may be ‘silent’. This means that although the defective gene is present, it does not result in any obvious symptoms.
Silent gene mutations can result in a ‘predisposition’ (tendency) to develop a disease which other individuals, not having the mutation, will never develop. A person may carry several of these mutations and not develop diseases. This is due to the large ‘reserve capacity’ of the body which allows it to maintain homeostasis using many compensating mechanisms.
When the pool of genes is mixed through mating, a new set of gene mutations may appear. This is called a ‘polygenetic disposition’. The offspring are again susceptible for disease which may be triggered by external factors (e.g. as seen in type 2 diabetes). Some people are robust and do not get sick upon the exposure whereas others are susceptible. We all know persons that catch colds every time they are exposed to viruses, whereas others are rarely sick.
Since it happens in a random way, it cannot be predicted.
Physiological factors
Age plays an important role for the normal (physiologic) function of the body. Our cells have a large reserve capacity from birth. This means they are capable of renewing themselves - they will be replaced if harmed or destroyed. However, the capacity for this varies from organ to organ and the total number of cell divisions in the body is limited. With a large amount of wear and tear, the pool of reserve cells may be used up. At this stage, disease may appear.
With age, the pool of available reserve cells also will decrease. This is the reason why the human lifespan is typically not more than 100 years. Figure 2 illustrates this relationship and how pharmacotherapy can affect disease progression.
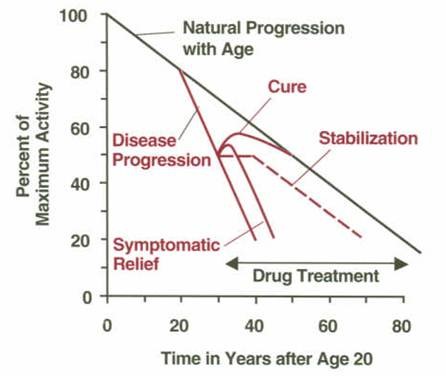
Figure 2: Progression of a given disease and influence of pharmacotherapy. The y-axis (vertical axis) shows the activity in the body function level in percentage of its maximum (at the age of 20 years). The activity level decreases with age (black curve). This decline in activity is accelerated in case of appearance of a disease (red curves). Pharmacotherapy can change the progress of the disease in the form of a cure, stabilisation and/or symptomatic relief (relief of symptoms).
Many physiological stressors lead to an unusual cell or organ deterioration which can cause disease. Some examples are as follows:
- High blood pressure is not a disease by itself. However, it may lead to changes in the blood vessels (vasculature), which can lead to thickening and hardening of the walls of the arteries (arteriosclerosis) and an increased risk for blood clots (thrombosis).
- High blood glucose levels (as seen with type 2 diabetes) can worsen kidney function, destroy a part of the eye called the ‘retina’ leading to blindness, and cause foot ulcers and pain.
- Overproduction of hormones and other mediators in the body can also cause problems. For example, in ‘thyrotoxicosis’ or ‘Basedows Disease’ the thyroid gland produces too much of the hormone ‘thyroxin’. Thyroxin stimulates metabolism, therefore causing an increased metabolism in those who have the disease. This will adversely affect many tissues, with the heart suffering first.
Defense mechanisms
We all have defense mechanisms in the body. Thus, if our immune system is very sensitive (‘hypersensitive’) due to genetic dispositions, it may run loose. Our immune system is there to protect us against infections and other exposures to toxic agents. Normally when it is working you feel ill, but at the same time it fights the infection and you recover to a normal state.
If you have a predisposition for disease such as an ‘allergy’ or ‘rheumatoid arthritis’, exposure to a toxic agent may trigger a chronic (long-term) state where the natural defence mechanism is continually active (it simply goes on and on).
In the case of rheumatoid arthritis this may be serious. The joint and bones become tender and swollen due to the ongoing immune reaction. This causes the joint and the nearby bones to be destroyed. Through pharmacotherapy it is possible to control the immune reaction and stop the disease signs (i.e. the damage to the joints and bones). However, it is still difficult to heal the underlying hypersensitivity.
- The medicines for this condition are called ‘anti-rheumatic’ medicines. They interact with targets on the immune cells which helps to inhibit or neutralise (i.e. stop) their activity. As long as the medicine is present in the body it acts as an ‘inhibitor’.
- However, when the medicine is removed, the immune cells become active again and the destruction of joint and bones continues.
This type of treatment is a balancing act. If over-treated the natural defense system is affected, and the patient becomes at risk of serious infections (e.g. sepsis).
Stress factors
A chronic (long-term) stress situation of physical, chemical or psychological origin may lead to disease. Some examples are shown below:
- Cancer caused by high and prolonged exposure to asbestos through polluted working conditions is an example of a physical stress situation. Asbestos fibres are very sharp and are the size of the cells that would normally help to remove them from the lung tissue. When breathed in, the body knows that the fibres are ‘foreign bodies’ and should not be there. This leads to a chronic (long-term) stress situation and the lung cells are eventually destroyed.
- An example of a chemical stress situation is the chronic (long-term) intake of large amounts of alcohol. The human liver is built to ‘detoxify’ or clear foreign substances, like alcohol. It can work harder to do this when required by increasing the enzymes involved in breaking down alcohol molecules. However, over years of drinking too much alcohol, the liver cells are broken down and become replaced with fat. This is called ‘fatty liver’. It can later lead to ‘liver cirrhosis’, where liver cells are replaced with scar tissue and ‘liver failure’, where the liver stops working.
- There is a direct link between the mind and the body. Thus, brain activity can activate hormone systems in the body. Psychological stress situations such as a high-pressure job or divorce may stimulate special brain cells to produce brain hormones. These hormones stimulate the ‘adrenal glands’ to produce stress hormones (called ‘corticosteroids’) which directly interact with cell processes all over the body. If the psychological stress is chronic (long-term), this could result in a weakened immune system. This makes the patient more likely to get infections or outbreak of diseases such as eczema, allergies or auto-immune reactions.
Susceptibility
The susceptibility (how likely you are) to catch a disease may vary from person to person. This may be related to genetic disposition either inherited or from a new gene mutation.
The influence of age through the reduction of the body’s reserve capacity has also been described. You are more likely to develop a disease with age, but this may vary from organ to organ. If you look at an important parameter such as blood pressure or glucose levels, these will be linked to an organ system (like skin, muscles, heart, kidney etc.). The green area in Figure 3 illustrates the reserve capacity of the organ (i.e. the capacity to cope with disturbances before obvious symptoms appear). This means that a given disturbance with no apparent effect in younger age may suddenly give rise to a disease when you get older (i.e. where the blue broken line passes into the red area). Treatment of the disease may bring the disturbance back to within the limit for normal well-being or homeostasis (the curved broken line starting from the medicine arrow).
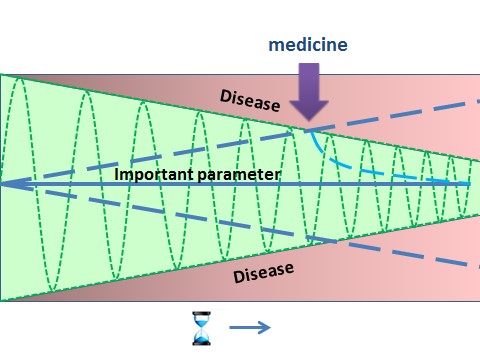
Figure 3: Illustration
of how susceptibility to catch disease increases with age. The body has an
inherent ability to correct any changes up to certain limits, without affecting
its homeostasis as a whole. Only when limits of correction are reached, disease
symptoms begin to appear. With age, the reserve capacity decreases. Thus the
green area represents the body’s reserve capacity as a function of age. The
green oscillation curve moves up and down and shows the range within which the
body can compensate changes (maximal allowed fluctuation), for example
during physical exercise. Introduction of medicines (arrow) brings the
important parameter (e.g. blood pressure, glucose level etc.) back within the
body’s reserve capacity.
The size of an individual’s reserve capacity will depend on their genetic makeup and the environmental conditions the person has been exposed to during their life. Some examples of environmental factors that will affect an individual’s reserve capacity are:
- Malnutrition with little access to proteins, vitamins and other nutrients. This is especially important in fetal development (development of the baby before birth) and in childhood.
- Poor hygiene, causing health threatening infections.
- Lack of regular physical activity.
- Excessive intake of calories and vitamins.
- Exposure to harsh conditions through working or living environments.