Mechanisms of disease
| Site: | EUPATI Open Classroom |
| Course: | Predisposing Factors and Underlying Mechanisms of Disease |
| Book: | Mechanisms of disease |
| Printed by: | Guest user |
| Date: | Saturday, 14 June 2025, 7:03 AM |
1. Basic Concepts
(This section is organised in the form of a book, please follow the blue arrows to navigate through the book or by following the navigation panel on the right side of the page.)
A disease is an abnormal physiological condition that affects part or all of an organism. It means that something has gone wrong with the normal body functions and/or processes. Diseases are linked with ‘symptoms’ and ‘signs’ – where a symptom is a manifestation of disease apparent to the patient himself, while a sign is a manifestation of disease that the physician perceives. The sign is objective evidence of disease; a symptom, subjective..
To determine the use of medicines for the treatment of diseases (pharmacotherapy), four concepts are important:
- Symptoms
- Diagnosis
- Mechanism described at a physiological and a molecular level
- Target responsible for the medicine’s action (in this context: organ, part, tissue that is to be affected by the medicine).
These are described in more detail below.
Symptoms
These are what the patient experiences as not being normal or worrisome (e.g. pain, bleeding, a lump felt somewhere, sweating a lot, dizziness, hearing problems etc.). The patient then presents these to the doctor. The doctor looks at these symptoms and tries to link them to a disease or a syndrome (where a collection of symptoms appear together). This allows the doctor to reach a diagnosis.
Diagnosis
The doctor forms a diagnosis (i.e. the disease or syndrome) on the basis of:
- the patient’s disease history and symptoms presented
- physical examination
- blood samples
- viewing of
internal structures of the body with X-ray, Computer Tomography (CT) or Magnetic Resonance (MR) scans.
Mechanism
Centuries of research have decoded many of the mechanisms that lead to the symptoms of disease and thereby to the diagnosis. These can be observed by:
- the naked eye
- physical and/or electrical measurements (e.g. of blood pressure, muscle strength, urine flow, size of a tumour, heart activity, etc.)
- physicochemical
measurements on blood samples or tissue samples (‘biopsies’).
Target
Identifying the mechanism of the disease helps us to understand what has gone wrong. It is important to then understand exactly which molecules (often proteins) are involved - this forms the ‘target’ for the primary action of the medicine. When medicines act on the target, they change the molecular processes, which in turn change the physiological processes. This therefore corrects the imbalance, which has led to the symptoms of the disease. The medicines do this through various interactions with molecules.
Knowing the mechanisms behind the observed symptoms of a disease is crucial to be able to initiate the right treatment.
What does the right treatment mean? Simply it
means re-establishing the correct balance in body function. This balance or
equilibrium is also called ‘homeostasis’. This describes the balance that
exists among all the components of the body. An adequate homeostasis means that
you are healthy and feeling vital (e.g. being full of energy when you wake up
in the morning) and you will not sense anything wrong with your body (i.e.
nothing aches or shows problems).
1.1. Example: Anaemia
Anaemia is a common disease, which is seen in all ages and in both genders. The sufferers will have the following symptoms:
- they will be pale
- the membranes (mucosa) which line the eyes and mouth are not red as usual
- the nails are pale
- the heart beats faster (higher pulse) than normal, in severe cases
- they will easily become short of breath when exercising
- they will feel tired and cold
- they are more likely to sweat - this is due to the extra work the heart is doing.
Anaemia means that less oxygen is transported in the body than required for normal functioning. The body tries to make up for this by using the following ‘compensation mechanisms’:
- Allowing the heart to pump more blood around the body. To do this, the heart beats faster and more blood is pumped at each heart beat (an increase in ‘stroke volume’). If this carries on for a long time, the heart will grow. This can be felt and seen on the naked chest as the ribs will rise higher than normal with each breath.
- Reducing the blood supply to organs that do not need as much oxygen (i.e. the skin and mucosa). This is the reason why patients with anaemia become pale and feel cold.
This is what can be observed with the naked eye (the macroscopic level).
Such compensation mechanisms also occur at the microscopic level - these things cannot be seen with the naked eye. One of the major causes of anaemia is not having enough iron in the body. Iron is important because it helps oxygen to bind to a special protein called ‘haemoglobin’ in the red blood cells. When iron levels are low, the body tries to make up for this by:
- releasing iron from reserves that exist in the liver and bone marrow.
- making the absorption of iron from food in the gut more effective by increasing the transport molecules in the mucosa of the intestines.
- improving the transport of iron to the bone marrow by increasing the concentration of ‘iron binding proteins’ in the blood. This is important because haemoglobin is produced in the bone marrow.
To bring the anaemic state back to normal (i.e. to re-establish the homeostasis) it is necessary to understand the cause(s) for the anaemia. Anaemia is a symptom and further diagnosis is needed. Through blood sampling, analysis and using a microscope to view samples (microscopy) it is possible to determine the cause. In special cases, it may be necessary to take a bone marrow biopsy. When the cause is established, the correct treatment can begin. If successful, the homeostasis will be restored, although continuous treatment with medicines (pharmacotherapy) may be necessary.
The number of possible causes for anaemia given below will probably surprise you:
Table 2: Causes and treatment options for anaemia
|
Causes |
Treatment |
|
Acute (sudden) loss of blood by heavy bleeding (e.g. from a trauma or injury) will lead to a reduced number of red blood cells. However, the remaining blood cells look normal. |
The bleeding should be stopped and the lost iron should be replaced through a blood transfusion.
|
|
Chronic (long-term) loss of blood (e.g. through heavy menstruation or bleeding from the intestines) will also reduce the number of red blood cells. However, as iron levels may have been low for a long time, the red blood cells may appear smaller, with less haemoglobin. |
|
|
Not taking in enough iron will resemble chronic blood loss, described above. |
Iron should be replaced by increased intake (e.g. in diet). |
|
Vitamin deficiency (e.g. vitamin B12 and folic acid) due to substandard food will cause large red blood cells with less haemoglobin. |
Vitamins should be replaced through injections with vitamin B12 or intake of folic acid. |
|
Infections with microorganisms called ‘protozoa’ (e.g. malaria) will acutely reduce the number of red blood cells. Microscopy will show the parasites in the blood. |
The infection with the malaria parasite should be treated with anti-malaria medicines. |
|
Lack of hormones that stimulate the production of red blood cells (e.g. if a protein called ‘erythropoietin’ (EPO) is lacking). |
Hormone replacement therapy should be used to restore normal levels of the hormone in the body. |
|
Presence of toxic compounds that bind to the red blood cells and destroy them. |
The toxic compounds should be removed (e.g. treatment with cytotoxic medicines, such as chemotherapy). |
|
An immune reaction where antibodies destroy red blood cells. This might be activated by medicines such as ‘sulphonamides’, or infections. |
The immune reaction should be stopped through treatment with anti-inflammatory medicines (corticosteroids). |
|
Displacement of dividing red blood cells from the bone marrow (e.g. by ‘leukaemia cells’). |
The leukaemia (a type of cancer) present at the same time should be controlled with cytotoxic medicines specific for the leukaemia cells. |
|
‘Sickle Cell Disease’ - a hereditary disease due to genetic mutations. In this illness the shape of the red blood cells is abnormal and fragile. |
Blood transfusions can be used to treat the symptoms. |
|
‘Aplastic anaemia’ – when the production of red blood cells is completely stopped, often for unknown reasons. |
Bone marrow transplant. |
Treatment will depend on the mechanism that causes the anaemia.
2. Disease
A disease may be caused by factors from an external source, such as infections, or it may be caused by problems with internal processes, such as auto-immune diseases.
In the following sections we describe the stages
and factors when going from an ideal healthy situation into developing a
disease.
2.1. Homeostasis
Homeostasis is the process which maintains the stability of the human body's internal environment in response to changes in external conditions. Besides ‘whole body’ homeostasis, the term is also used to describe particular processes or systems like the regulation of body temperature.
An analogy is the knots in a fishing net. See Figure
1.
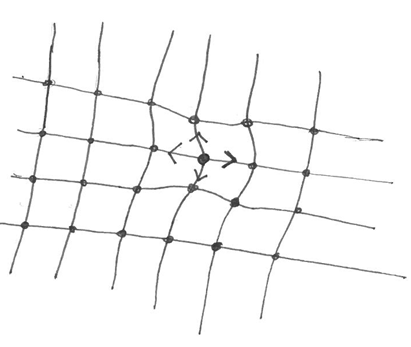
Figure 1: Illustration of the fishing net analogy
What can we learn from this analogy?
- Pulling locally on one of the knots changes the position but does not destroy the overall net structure. This reflects the whole body and the individual systems within it.
- Local changes (e.g. by lifting one of the knots) in a fishing net will not only give rise to the change of the position of the knot in question but also of some of the neighbouring knots. This shows that it is not possible to change a single parameter without influencing the surrounding system, just as in the body.
- Releasing the knot of the net brings the net back to its original position. You could think of this like pharmacotherapy, where treatments and medicines help to restore the balance in the body.
A medical doctor studies the groups of symptoms that characterise a disease (called a ‘symptom complex’) of all types of diseases. They do this in a similar way to that described in Example 2 for anaemia, but in much more detail. The space given in this section is too limited to go through all diseases. Instead we will focus in a systematic way on the principles behind disease mechanisms and how these mechanisms can be controlled through intervention in the form of pharmacotherapy.
2.2. Natural History
First of all, it is important to understand that diseases have a natural history of progress within the body. Diseases do not always develop in a linear way. Sometimes there may be ‘jumps’, such as worsening or improvement in health status. For the doctor as well as the patient, it is important to understand this to be able to monitor the effect of a given pharmacotherapy or treatment.
Often disease progression takes place over a long time before any obvious symptoms can be seen. This is due to the organism being able to correct any changes up to certain limits, without affecting the system’s homeostasis as a whole. It is only when these limits are reached that disease symptoms become evident.
Pharmacotherapy can reverse or stop the process, but not repair any destroyed tissues.
As seen in the case with anaemia, the underlying causes for the symptoms are important. The causes and origin of the disease are in medical terms described by the word ‘aetiology’. A patient can be treated either through lifestyle changes and/or through medical intervention such as surgery or pharmacotherapy.
2.3. Factors Causing a Disease
The factors causing a disease can be categorised into the following groups:
- External factors
- Internal factors
- Physiological factors
- Stress factors
- Susceptibility
These are described in more detail below.
External factors
The external factors causing imbalances or diseases include:
- Microbes (bacteria and viruses) and parasites (e.g. malaria and amoebae)
- Injuries (accidents)
- Environmental impact during an individual’s lifetime - this is also linked to personal habits mentioned as ‘lifestyle’, e.g. food and fluid intake and physical exercise.
Internal factors
These are also known as ‘genetic factors’. If the genes of the sexual organs (i.e. egg or sperm) are permanently harmed by external factors, a change in the genes (‘mutation’) can appear. This may cause ‘monogenetic disease’ in the offspring - this is disease caused by a single defective gene. Sometimes this is easily observed (e.g. in dwarfism, where people are short in stature), where for others it may be ‘silent’. This means that although the defective gene is present, it does not result in any obvious symptoms.
Silent gene mutations can result in a ‘predisposition’ (tendency) to develop a disease which other individuals, not having the mutation, will never develop. A person may carry several of these mutations and not develop diseases. This is due to the large ‘reserve capacity’ of the body which allows it to maintain homeostasis using many compensating mechanisms.
When the pool of genes is mixed through mating, a new set of gene mutations may appear. This is called a ‘polygenetic disposition’. The offspring are again susceptible for disease which may be triggered by external factors (e.g. as seen in type 2 diabetes). Some people are robust and do not get sick upon the exposure whereas others are susceptible. We all know persons that catch colds every time they are exposed to viruses, whereas others are rarely sick.
Since it happens in a random way, it cannot be predicted.
Physiological factors
Age plays an important role for the normal (physiologic) function of the body. Our cells have a large reserve capacity from birth. This means they are capable of renewing themselves - they will be replaced if harmed or destroyed. However, the capacity for this varies from organ to organ and the total number of cell divisions in the body is limited. With a large amount of wear and tear, the pool of reserve cells may be used up. At this stage, disease may appear.
With age, the pool of available reserve cells also will decrease. This is the reason why the human lifespan is typically not more than 100 years. Figure 2 illustrates this relationship and how pharmacotherapy can affect disease progression.
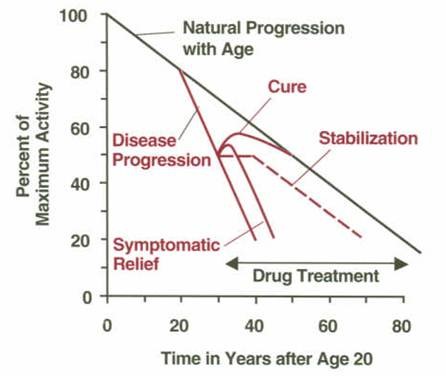
Figure 2: Progression of a given disease and influence of pharmacotherapy. The y-axis (vertical axis) shows the activity in the body function level in percentage of its maximum (at the age of 20 years). The activity level decreases with age (black curve). This decline in activity is accelerated in case of appearance of a disease (red curves). Pharmacotherapy can change the progress of the disease in the form of a cure, stabilisation and/or symptomatic relief (relief of symptoms).
Many physiological stressors lead to an unusual cell or organ deterioration which can cause disease. Some examples are as follows:
- High blood pressure is not a disease by itself. However, it may lead to changes in the blood vessels (vasculature), which can lead to thickening and hardening of the walls of the arteries (arteriosclerosis) and an increased risk for blood clots (thrombosis).
- High blood glucose levels (as seen with type 2 diabetes) can worsen kidney function, destroy a part of the eye called the ‘retina’ leading to blindness, and cause foot ulcers and pain.
- Overproduction of hormones and other mediators in the body can also cause problems. For example, in ‘thyrotoxicosis’ or ‘Basedows Disease’ the thyroid gland produces too much of the hormone ‘thyroxin’. Thyroxin stimulates metabolism, therefore causing an increased metabolism in those who have the disease. This will adversely affect many tissues, with the heart suffering first.
Defense mechanisms
We all have defense mechanisms in the body. Thus, if our immune system is very sensitive (‘hypersensitive’) due to genetic dispositions, it may run loose. Our immune system is there to protect us against infections and other exposures to toxic agents. Normally when it is working you feel ill, but at the same time it fights the infection and you recover to a normal state.
If you have a predisposition for disease such as an ‘allergy’ or ‘rheumatoid arthritis’, exposure to a toxic agent may trigger a chronic (long-term) state where the natural defence mechanism is continually active (it simply goes on and on).
In the case of rheumatoid arthritis this may be serious. The joint and bones become tender and swollen due to the ongoing immune reaction. This causes the joint and the nearby bones to be destroyed. Through pharmacotherapy it is possible to control the immune reaction and stop the disease signs (i.e. the damage to the joints and bones). However, it is still difficult to heal the underlying hypersensitivity.
- The medicines for this condition are called ‘anti-rheumatic’ medicines. They interact with targets on the immune cells which helps to inhibit or neutralise (i.e. stop) their activity. As long as the medicine is present in the body it acts as an ‘inhibitor’.
- However, when the medicine is removed, the immune cells become active again and the destruction of joint and bones continues.
This type of treatment is a balancing act. If over-treated the natural defense system is affected, and the patient becomes at risk of serious infections (e.g. sepsis).
Stress factors
A chronic (long-term) stress situation of physical, chemical or psychological origin may lead to disease. Some examples are shown below:
- Cancer caused by high and prolonged exposure to asbestos through polluted working conditions is an example of a physical stress situation. Asbestos fibres are very sharp and are the size of the cells that would normally help to remove them from the lung tissue. When breathed in, the body knows that the fibres are ‘foreign bodies’ and should not be there. This leads to a chronic (long-term) stress situation and the lung cells are eventually destroyed.
- An example of a chemical stress situation is the chronic (long-term) intake of large amounts of alcohol. The human liver is built to ‘detoxify’ or clear foreign substances, like alcohol. It can work harder to do this when required by increasing the enzymes involved in breaking down alcohol molecules. However, over years of drinking too much alcohol, the liver cells are broken down and become replaced with fat. This is called ‘fatty liver’. It can later lead to ‘liver cirrhosis’, where liver cells are replaced with scar tissue and ‘liver failure’, where the liver stops working.
- There is a direct link between the mind and the body. Thus, brain activity can activate hormone systems in the body. Psychological stress situations such as a high-pressure job or divorce may stimulate special brain cells to produce brain hormones. These hormones stimulate the ‘adrenal glands’ to produce stress hormones (called ‘corticosteroids’) which directly interact with cell processes all over the body. If the psychological stress is chronic (long-term), this could result in a weakened immune system. This makes the patient more likely to get infections or outbreak of diseases such as eczema, allergies or auto-immune reactions.
Susceptibility
The susceptibility (how likely you are) to catch a disease may vary from person to person. This may be related to genetic disposition either inherited or from a new gene mutation.
The influence of age through the reduction of the body’s reserve capacity has also been described. You are more likely to develop a disease with age, but this may vary from organ to organ. If you look at an important parameter such as blood pressure or glucose levels, these will be linked to an organ system (like skin, muscles, heart, kidney etc.). The green area in Figure 3 illustrates the reserve capacity of the organ (i.e. the capacity to cope with disturbances before obvious symptoms appear). This means that a given disturbance with no apparent effect in younger age may suddenly give rise to a disease when you get older (i.e. where the blue broken line passes into the red area). Treatment of the disease may bring the disturbance back to within the limit for normal well-being or homeostasis (the curved broken line starting from the medicine arrow).
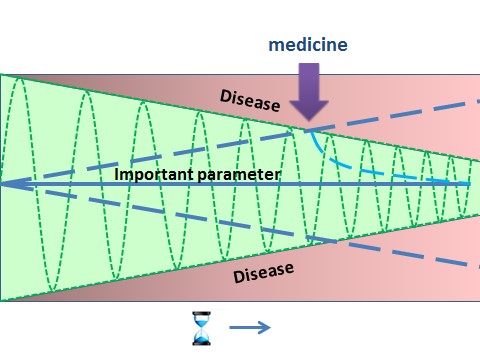
Figure 3: Illustration
of how susceptibility to catch disease increases with age. The body has an
inherent ability to correct any changes up to certain limits, without affecting
its homeostasis as a whole. Only when limits of correction are reached, disease
symptoms begin to appear. With age, the reserve capacity decreases. Thus the
green area represents the body’s reserve capacity as a function of age. The
green oscillation curve moves up and down and shows the range within which the
body can compensate changes (maximal allowed fluctuation), for example
during physical exercise. Introduction of medicines (arrow) brings the
important parameter (e.g. blood pressure, glucose level etc.) back within the
body’s reserve capacity.
The size of an individual’s reserve capacity will depend on their genetic makeup and the environmental conditions the person has been exposed to during their life. Some examples of environmental factors that will affect an individual’s reserve capacity are:
- Malnutrition with little access to proteins, vitamins and other nutrients. This is especially important in fetal development (development of the baby before birth) and in childhood.
- Poor hygiene, causing health threatening infections.
- Lack of regular physical activity.
- Excessive intake of calories and vitamins.
- Exposure to harsh conditions through working or living environments.
3. Targets for action of medicines
From the descriptions given above it appears that genetic disposition, lifestyle and environmental factors may all influence the development of diseases at many different locations in the body. If we understand the molecular mechanisms behind various diseases (i.e. what has gone wrong at the level of the cells), we can develop medicines that may reverse the harm caused by a disease. This brings us to the question: which molecules in the body are targets for medicines.
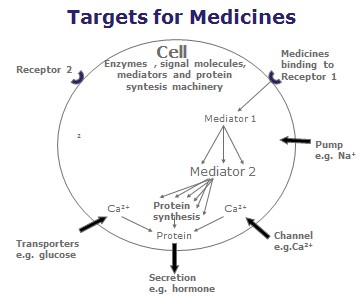
Figure 5: a diagram of a cell showing some targets for the actions of natural ligands (see next section ‘Receptors’ for description) and medicines. The cell machinery is made up of signal molecules, enzymes, mediators and molecules for protein synthesis. By activating a few receptors, this can cause a ‘cascade reaction’ (a series of several reactions) inside the cell. The medicine can work with the cell to produce the desired effect. For example, by adding a few medicine molecules, the cell can produce or ‘secrete’ many molecules of the final product (e.g. a hormone). Medicines can also bind to ‘channels’ and ‘pumps’ on the cell surface, to alter how the cell works and what it secretes.
3.1. Receptors
The main target is ‘receptors. These are protein molecules found on the surface of the cell. They are often the first stage of the molecular processes, which lead to reactions within the cell. These reactions may cause symptoms of a disease. See Figure 5. A receptor sits on the surface of a cell. It receives a chemical signal when another molecule called the ‘ligand’ binds to it. A ligand is a small molecule that triggers signals by binding to receptors.
A medicine behaves like a ligand. Binding only takes place when the two molecules fit in each other like ‘the key to a lock’. The binding of the ligand causes the receptor to send a message to other molecules inside the cell - causing the cell to start working. It can be a chemical reaction like secretion, a mechanical reaction, such as a change of cell shape. This might in turn bring about cell division or a movement (displacement) of ions causing an electric impulse from that cell (called an action potential).
By interacting with the first stage of the cascade reaction (i.e. the receptor), it is possible to change the end process. When medicines are used, they are designed to act on a large number of molecules with a minimum amount of medicine. This is so that a large amount of secretion (e.g. a hormone like insulin or enzymes for digestion like pepsin in the stomach) can be produced.
3.2. Transporter molecules
Other important targets include ‘transporter’ molecules, which serve either as channels or pumps. See Figure 5. These protein molecules also sit on the cell surface. They control the movement of salts (ions), metabolites, nutrients and medicines across the cell membrane. Ions like ‘calcium’ (Ca++) may also assist secretion, as above.
Transporters are also very important for the ‘absorption’ process in the gut - this is how nutrients from your food get into your blood. Again they control the movement of molecules from the body’s external surface to the inner compartments. They are crucial for the body’s homeostasis as they help to increase or decrease the concentration of metabolites and ions in the body. In the case of disease, it is possible to treat specific transporters through medicines that inhibit (decrease) or promote (increase) these processes, to restore homeostasis.
Since cell membranes do not allow water soluble substances to pass, transporters serve as ‘gates’ for what enters and leaves the cell. They therefore have an influence on the activity of the cell. An example of medicines that act on transporter molecules are ‘diuretics’. They control the excretion of salts (ions) via pumps in the kidney cells - this helps the body to remove excess salts and water through the urine.
3.3. Enzymes
A third group of medicine targets are ‘enzymes. These proteins facilitate (catalyse) chemical processes within the body (e.g. in body fluids such as ‘blood plasma’). The hormone GLP-1 is a good example. GLP-1 assists the secretion of insulin, which is involved in reducing blood glucose levels. However, GLP-1 can be quickly broken down in blood plasma by a specific enzyme. By introducing a medicine that inhibits this enzyme, the natural GLP-1 molecule is active long enough to work. This can help to reduce symptoms linked to high blood sugar levels.
3.4. Missing ligands
Finally, in some diseases the target is undisturbed and intact, but the internal ligand that binds to the target is missing. Therefore, homeostasis cannot be achieved. The ligand could be a small molecule like a metabolite, a hormone, a transmitter (e.g. dopamine), a vitamin, a nutrient (e.g. amino acids) or an ion (e.g. iron). It could also be a large molecule like a hormone (e.g. insulin, thyroxin, corticosteroids). If it is possible to produce the ligand, ‘substitution therapy’ can be used. This therapy replaces the natural ligand in the body. For example, use of synthesised insulin in the treatment of diabetes. This can also apply to vaccines and cells (e.g. red blood cells (by transfusion) or stem cells (by transplantation)).
4. Medicines interaction with target
If a target for the treatment of a given disease has been identified through comprehensive experiments in the discovery phase, the developer of the medicine can still not be sure that the medicine being developed will show the desired interaction with the target when used in patients. In fact, when used on patients the most important thing for the developer to see is effects against the disease (i.e. showing ‘efficacy’ - that the medicine works). The medicine can have the expected effect on the target, but the symptoms of disease may remain unchanged. This may be due to other mechanisms in the body that override the effect of the medicine on the target. They take over for the pathway that has been affected by the medicine.
5. Clinical Endpoints
To ensure that the medicine has the desired effect on the disease, clinical trials with patients who have the disease are conducted. Again, it is not enough to ensure that the target activity is changed, since the symptoms of the disease could still persist. It is therefore important to determine the effect of the treatment in the patients. These are measured and known as ‘clinical endpoints’ as defined in the trial protocol. Clinical endpoints could be:
- the number of bone fractures in a given period - after starting treatment for ‘osteoporosis’ (a condition where patients have fragile bones)
- the length of migraine attacks - after the medicine for migraine has been given
- blood factors important for oxygen transport returning to normal levels - after treatment for anaemia has started
- number of verified ‘acute myocardial infarctions’ (heart attacks) or even death - in patients receiving preventative treatment for thickening of the arteries (arteriosclerosis).
It is important that the endpoints measured are objective (i.e. unbiased) and allow for quantification (i.e. they are countable). When an effect is seen by such measurements, the Regulatory Authorities involved in granting the Marketing Authorisation of the medicinal product can be sure that the medicine is effective. Thus, it is only through the conduct of clinical trials that evidence for the benefit of a medicine can be provided.
The other, and equally important aspect, is the safety of the medicine. Based on these two factors the benefit (efficacy) and risk (safety) of a medicine can be evaluated - this is called the benefit-risk relationship. The medicine will only be allowed on the market if the benefits are higher than risk, i.e. there is a positive benefit-risk relationship.
6. Summary
Behind the symptoms of disease which lead to a diagnosis, there is a row of processes (metabolic pathways) involving many molecules. Sometimes, for various reasons, these processes or molecules stop working or do not work as they should. This leads to imbalances of the body’s homeostasis. The anaemia case (Example 2) shows that there are many different molecular processes behind a given symptom. This means that different pharmacological treatments are needed to cure the underlying disease or relieve the symptoms. Factors causing disease vary between individuals. This is due to different genetic dispositions and the body’s reserve capacity to maintain homeostasis. This means that external factors like microbes, chemical or psychological stressors may result in disease in some individuals but not in others.
It is the purpose of pharmacotherapy to restore homeostasis. This is done by identifying key molecules in the processes that are not working and by correcting their activity, either through inhibition, promotion or by supplementing components that are missing. However, to ensure that a medicine is effective, it is not enough to show that it acts on the target. It also needs to be shown to reduce the symptoms of the disease. This is done by measuring the effect on clinical endpoints in clinical trials with patients.